How one pathogen evades the immune system
11 Jan 2021
An LMU research team has uncovered a mechanism that enables the parasite that causes sleeping sickness in humans to escape the immune system.
11 Jan 2021
An LMU research team has uncovered a mechanism that enables the parasite that causes sleeping sickness in humans to escape the immune system.
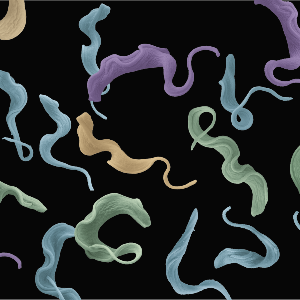
T. brucei causes sleeping sickness. | © Meyer-Natus/Siegel
Our immune system is never idle. Their task is to detect and eliminate invasive pathogens, and they have no time to lose. The adaptive immune system identifies infectious organisms by recognizing foreign proteins on the surfaces of bacteria, viruses and unicellular protozoans. The interaction of these antigens with immune cells triggers a series of downstream events, which in most cases leads to the elimination of the pathogen.
But pathogenic organisms have developed strategies that enable them to escape detection by the immune system, and the strategies employed by remotely related organisms are often remarkably similar to each other. One way of confusing the immune system is to increase the structural heterogeneity of the antigens it encounters. In bacteria,pathogenic yeast and parasites this can be done by randomly activating different members of gene families, which code for non-identical versions of the proteins expressed on their surfaces. This strategy essentially allows the infectious agent to duck under the immune system’s radar. By doing so, it significantly increases the likelihood that the invader will survive to establish an infection, and has a better chance to be transmitted to new hosts. If pathogens alter their surface proteins rarely – or too often – the white blood cells that are responsible for recognizing them have a much easier task. Nicolai Siegel (Professor of Molecular Parasitology at LMU) and his group, in collaboration with colleagues at the University of Dundee, have now elucidated an important step in the mechanism that controls surface-antigen variation.
While Siegel’s team is part of the department of Experimental Parasitology and affiliated with the Faculty of Veterinary Medicine at LMU, it makes use of laboratories located in the Physiological Chemistry section of the Biomedical Center (Faculty of Medicine). "This arrangement greatly facilitates scientific discussion and interdisciplinary exchanges,” he says.
His team works with the unicellular organism Trypanosoma brucei. There are several reasons for this. T. brucei causes sleeping sickness. It is transmitted by the tsetse fly, and it presents a threat to millions of people in 36 African countries south of the Sahara. From a scientific point of view, however, this species has become a model system for the study of antigen variation in pathogens, and has therefore been widely studied.
The genome of T. brucei includes more than 2000 genes that code for variant forms of the major protein expressed on its surface. In each individual cell, only one of these genes is activated – and it directs the production of a single surface-protein variant. “The pathogen must therefore ensure that only one of these genes ¬– not a few, and certainly not all – of the genes for surface proteins are expressed at any given time,” Siegel explains. “We have now identified the mechanism that guarantees that the product of only one of these genes is expressed.”
Notably, T. brucei does not possess complex arrays of regulatory genomic sequences – such as enhancers – which are involved in determining the set of genes that are transcribed from the genomic DNA into messenger RNAs (mRNAs) at any given moment. These mRNAs subsequently direct the synthesis of the corresponding proteins. “The control mechanism that we have discovered appears to achieve the required selectivity by differentially regulating mRNA maturation,” Siegel says. This in turn is accomplished by chemically modifying specific mRNAs, which prevents them from being rapidly destroyed.
The authors of the new study have identified a three-dimensional structure in the nucleus of T. brucei that serves as a separate compartment, in which the mRNA molecules that encode the cell’s single surface protein variant are modified. As a result, they avoid rapid destruction, and therefore survive long enough to produce the protein in the required amount. Conversely, when one of the proteins that contribute to the assembly of this compartment was inactivated, several different surface antigens were synthesized at the same time.
“So we now know why only one surface antigen is successfully expressed,” says Siegel. Moreover, these new results have implications that transcend their importance for basic research. “If we could control the process that leads to the switching of surface antigens, it might be possible to inhibit it,” he muses. And indeed, in the medium term, he sees in this possibility a new approach to the elimination – by the body’s immune system – of pathogens that depend on this form of antigenic variation.